“This. Is. Traumatic.”
That’s the assessment of one UW Health nurse, shared in a Facebook message with Madison365, of the current COVID situation in Wisconsin’s hospitals.
The novel coronavirus pandemic has Wisconsin in the grip of the highest infection rate in the country — 35.9 percent of people tested in the past week have tested positive, and 43 have died every day, on average. Wisconsin will have lost a total of 2,500 citizens to the virus by the end of the day Thursday, and some models indicate it could lose another 2,500 by the end of the year. Legislative Republicans and conservative-leaning organizations like Wisconsin Manufacturers and Commerce, the Tavern League of Wisconsin and Right to Life Wisconsin have sued to stop every measure Governor Tony Evers has attempted, including the “Safer at Home” order put in place last spring. The legislature hasn’t convened since April.
Assembly Speaker Robin Vos told the Milwaukee Journal Sentinel that he hasn’t spoken with Evers since May, but that he called and left Evers a message Tuesday night, after Evers addressed the state on a day 7,075 new cases were confirmed and 66 deaths were reported — both new records.
Also Tuesday, more than 2,000 people were hospitalized with COVID in Wisconsin, placing the state’s health care workers in a dire situation.
Like several others who reached out to Madison365, the UW Health nurse asked to remain anonymous, fearing of on-the-job reprisals for speaking publicly. The nurse said it’s not only the specialized COVID units feeling the pressure.
“All units are feeling the pain,” the nurse wrote. “The complexity of care and shortage of staff for non COVID patients, and being pulled out of your unit to work a specialty you’re not familiar with, has RN’s and CNA’s exhausted and burning out. The longer it drags on for, the more staff that get sick, the more losses we face, the harder it gets.”
A UW Hospital certified nursing assistant (CNA) echoed that sentiment, also in a Facebook message to Madison365. The CNA said workers at UW Hospital watched in horror what was happening in Italy and New York early in the spring.
“We didn’t speak of our anxiety and fear directly to each other, we just knew we were all on the same page, we didn’t have to say it,” the CNA said. “The first wave passed and we all settled into our new normal. The fall neared and we knew things would get worse. I don’t think any of us were really prepared for this second wave. There is such a mix of emotions now. We are scared of what is happening. Our beds are filling up fast. We were short staffed before covid and now we are even more short staffed because we have more patients and hundreds of staff out for covid-related reasons. We are frustrated with our government and the general public for fighting every attempt to ease this pandemic. Anger when we hear the conspiracy theorists claiming healthcare workers are falsifying death certificates and diagnoses to get more money. We are all so unsure of what tomorrow, or next week, or next month might look like. We are physically and emotionally exhausted.”

SSM Health Regional Vice President Veronica Scott-Fulton, the chief nursing executive for all of SSM’s seven hospitals and 85 clinics in Wisconsin, said nurses often work 12-hour shifts, and have a hard time turning off when they leave work.
“One of the things about healthcare is that it is all-encompassing,” she said. “It’s not really something you can turn on and off. Even for me, when I go to church, I’m a nurse. When I go to family and friends, I’m a nurse. When I’m in my circle of friends, I’m a nurse. it is an ever-present overwhelming feeling.”
She said the relentless nature of the pandemic takes a toll.
“It has been overwhelming. It’s totally exhausting. It almost makes you feel a bit diminished, not just as a nurse, but as a person,” she said.
More emotional trauma stems from the fact that patients can’t have family at their bedside, due to the virulent nature of the disease.

“It’s always sad when you lose patients,” said Ashok Rai, CEO of Prevea Health in Green Bay. “But a lot of these patients have been with us for one, two, three, four weeks and then can pass away and they haven’t had their family at the bedside. So our frontline staff become their family at the bedside … The staff essentially adopts them as their family. And so it creates a lot of stress and sadness amongst them on top of all the other pressures they have.”
Isolation from family also impacts the patients physically, Scott-Fulton said.
“There’s such a sense of isolation it makes it more difficult,” she said. “We feel that it actually extends the healing process. We feel that it actually leads to more system failures because they are not in a space where they feel totally safe with family members present that they know very, very well.”

“I am hearing from staff all across Wisconsin that they are feeling tired and at times overwhelmed,” said SSM Regional President Damond Boatwright. “I think in the early days of the pandemic, there was anxiety about the unknown. We’re now entering the ninth month of our pandemic response, which is now presenting new, clear and present stressors for our staff.”
High water mark
In addition to the toll on healthcare staff, the pandemic is putting a strain on capacity at healthcare facilities and their resources.
“The question of capacity was a non-issue four weeks ago, when we had approximately about 20 patients that were hospitalized for COVID,” Boatright said. “Today, it’s 98 patients hospitalized with COVID, today 98 patients are in the hospital, hospitalized with COVID and we are reaching a high water mark for ICU capacity right now.”
Those are 98 patients in SSM’s hospitals. The total number of inpatient COVID cases in Wisconsin as of Wednesday afternoon was 2,102. Those aren’t ordinary patients, Rai said.
“It’s an extra set of patients that are probably two to three times harder to take care of. So an extra 10 COVID patients is like 30 extra patients,” Rai said. “From a time standpoint, just the amount of personal protective equipment you have to put on and take off during that time period, it’s resource intensive, it’s time intensive. Our systems weren’t designed to take care of an extra 50-plus COVID patients in a given day, depending on the hospital you’re in. And then you take two ICU nurses out of circulation (if they test positive), that means everybody else has to step up.”
Complicating matters are staff shortages due to COVID infection among health care providers. Boatwright said 748 of SSM’s over-14,000 employees had tested positive — a relatively small number — but 120 are currently out while they await test results and undergo observation.
Scott-Fulton said SSM is “at a good place” in terms of capacity, but an SSM orthopedic nurse told Madison365 that several rooms on the orthopedic floor had been converted to COVID rooms, and some were occupied by COVID patients as of Tuesday.
“If we receive an additional increase of patients requiring hospitalization and ICU care, then we’re going to have to depend on other facilities outside of our own to take care of those patients,” Boatwright said.
“Heroes”
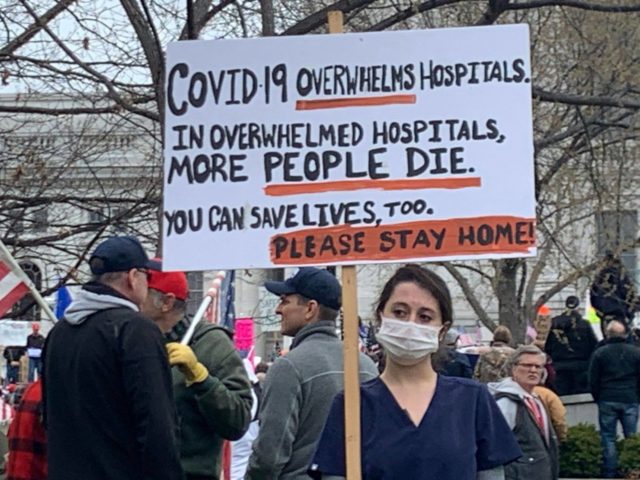
All the health care leaders Madison365 spoke with sang the praises of the front-line providers, and urged the public to do more to support them — primarily by working together to slow the spread of the virus.
“I think the staff is doing their very best to hold it together,” Boatwright said. “I applaud their resilience during the face of this unprecedented pandemic, but I worry for them and for us as a community in terms of how long our caregivers can continue in this fashion. I think what’s disheartening for folks now is we haven’t really gotten into the winter yet, and we already are starting to exceed our capacity.”
Rai said he’d like to see the community show those health care workers some support.
“In the spring, everybody was on healthcare’s side. We tied blue ribbons around trees because we wear blue scrubs and the staff felt really well supported,” he said. “They’re working very hard to take care of the community and they would like the community to help them out.”
He said health care providers find it “demoralizing” when they see people attending large gatherings or refusing to wear masks indoors.
“We also wear a seatbelt when we’re in cars,” Scott-Fulton said. “I mean, it’s okay. Just put that mask on.”
Boatwright said you can help support health care workers by simply staying healthy.
“Continue or start wearing a mask and find creative and virtual ways to connect with your loved ones and your friends. Get a flu shot,” he said. “Please get a flu shot because if we can reduce the number of people who acquire the flu and get hospitalized and we can reduce the number of people who get COVID positive, that makes it workable for us to be able to get through this particular crisis. Wash your hands, wash your face.”
Rai said he doesn’t feel that politics or policy is the place to turn.
“I’m not a big believer that policy is the solution,” he said. “I mean, I think we do need policies to re-enforce, but especially in the State of Wisconsin, every policy is going to get litigated. So instead of doing that, if we can get more of the community to just understand … maybe putting the politics aside and say, ‘All right, let’s team up, let’s get control over this for the next four to six months, and then we’ll all get our lives back together.’ Those are things that I think are going to work more than one politician versus another politician. Unless we can get all the politicians to say the same thing, it’s probably not going to be advantageous.”
Hope
Boatwright said he sees hope in a community that he perceives wanting to move beyond divisive politics.
“I think people want more community than they’ve had before. Social distancing and being separated from people, I think people realize they want to be connected. I’m hopeful that I’ve seen a lot of in the midst of all of this, I’ve seen more of a yearning for connectedness and people coming together than I saw previously, leading up to it.”
Rai sees hope in his own staff.
“What probably gives me hope the most has been those nurses in the ICU, they’re tired, they’re frustrated, and yet they show up the next day with a smile ready to do battle,” Rai said. “And they are my heroes. They are incredible people. If you can’t see hope in their eyes, then I don’t know where you’re going to find hope.”