No pandemic was going to get in the way of Iliana Arcelay’s dream to become a nurse.
No pandemic was going to get in the way of Iliana Arcelay’s dream to become a nurse.
Plenty of life events had already delayed the dream for the mother of four, who grew up in Milwaukee and returned to the area eight years ago after a stint in Florida.
“Nursing has been something I’ve wanted to do since I was a kid,” she said in a recent interview. But when her first child came along shortly after high school, she opted to focus on being a mom – a career she continued when another child arrived, followed by a set of twins. She worked a successful real estate career around her motherhood duties, but going back to college for a four-year degree was never going to fit.
“We as parents don’t have much time. As a single mother, I have to make ends meet,” she said.
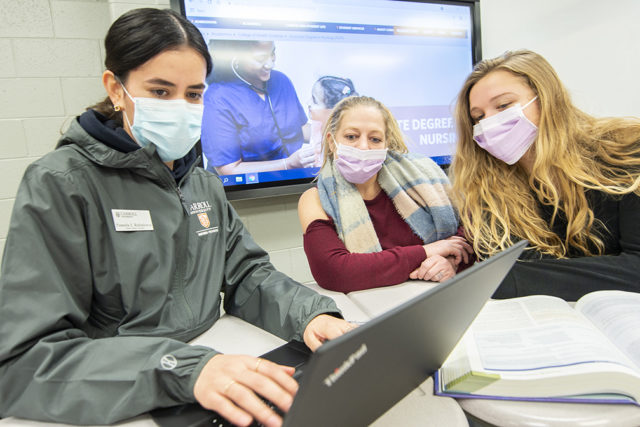
Then one day a bit over a year ago, Arcelay’s mom was riding past United Community Center in downtown Milwaukee and saw a sign for a new two-year nursing program, run at UCC by Carroll University. The application deadline had passed, but Arcelay emailed anyway; that was on a Friday, and by Monday she’d taken a tour of the facility and submitted an application.
Arcelay is now a member of the first cohort of Carroll’s brand new Associate Degree in Nursing (ADN) program, the university’s effort to address a significant and worsening shortage of registered nurses in the healthcare industry.
“Silver tsunami”
The nursing shortage is nothing new, and was not caused by the pandemic. It’s been an urgent topic of conversation among healthcare leaders and educators for several years; planning for the Carroll University ADN program began in 2016.
Like many other issues, however, the pandemic accelerated and exacerbated the problem.
Dr. Teresa Kaul, the chair of Carroll’s Nursing Department, said the state’s institutions are putting out about 3,700 new nurses every year – that includes registered nurses who earn associates, bachelors and masters degrees.
And that’s not nearly enough.
By 2025 – just three years from now – experts say the state will need no fewer than 9,800, more than a 250% increase from the current level, Kaul said.
“We’ll need 16,700 (annual nursing graduates) by 2030. We need 23,000 by 2035 and 27,700 by 2040,” Kaul said, citing Wisconsin Center for Nursing statistics.
The demand is driven largely by an aging population.
“We have a silver tsunami, as they call it here. We have an aging population in the state of Wisconsin that’s gonna blow up on us really quickly for our Baby Boomers,” she said. “We are going to need so much healthcare for these folks, that it’s going to be really scary.”
That also means an aging workforce in nursing that are retiring “in droves,” Kaul said.
The pandemic made the shortage worse by driving many out of the profession entirely.
“There’s been some real moral injury to our nurses,” Kaul said. “They’ve never had to face some of the things that they faced in nursing. We teach our nurses about patient centered care, taking care of the one patient. But when you’re asking nurses to make choices between patients and who gets treatment and who doesn’t, when you’re short on PPE, and you’re short on ventilators … our soldiers go through that and our soldiers come back with PTSD. How could you expect the nurses working out there in those kinds of environments not to have some long lasting effects?”
All of that means, though, that nursing jobs will always be available – which is one of the motivators for Arcelay to join Carroll’s ADN program.
“(The pandemic) helped me to push to have to survive. Things are falling apart around us. That just helped me to say, you know, I just need something that’s more stable,” she said. “Nursing is something that will never go away. The pandemic did show us that … it’s not going anywhere. No matter what, there are jobs and they’ll be there. … I think if anything, (the pandemic) made me want to pursue it more.”
Removing barriers to nursing school
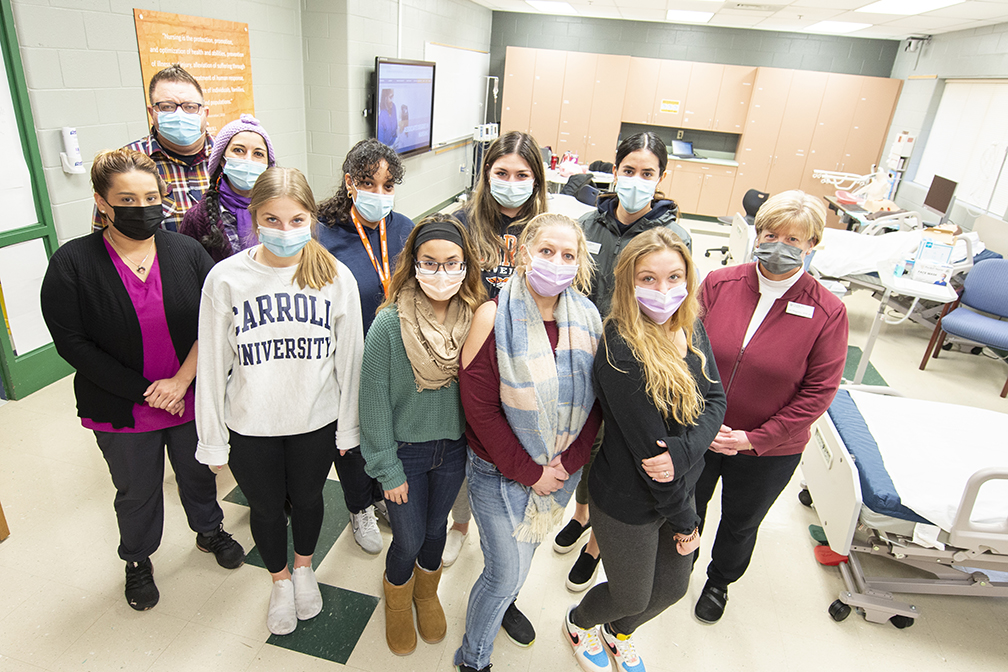
Kaul said Carroll’s administration recognized two facts that informed the creation of its new ADN program: first, the nursing profession needs to diversify, and second, many people who would make wonderful nurses can’t access a four-year university education.
“Nursing is in dire need of diversity,” Kaul said, which is one reason the new ADN program prioritizes admission of bilingual students. “We know that the outcomes and health outcomes of patients are better when cared for by people of their own culture. That’s really one of the main reasons why we want to provide people from that culture an opportunity to enter into a wonderful profession. And I think that hasn’t always been afforded to them.”
With grant funding and working closely with UCC staff, Carroll designed the program – the first associate’s degree program in the university’s 176-year history – to meet the needs of students, aspiring nurses, and community members where they are.
“(UCC) felt that a number of the people in that community, some of the folks coming out of the schools there would love to go to a four-year institution, but for financial reasons, for cultural reasons, they would prefer to stay in the community,” Kaul said. “It actually would address both the shortage of nursing, because we need more people in nursing. But we also want to increase diversity. So we kind of want those two to go hand in hand.”
“In my clinical rotations, I’m seeing (the need for diversity) firsthand,” Arcelay said. “There are people that you walk into the room and the minute that they see that you speak their language, it’s like a breath of fresh air. They’re able to let down their guards, and you see a difference in the way that they’re communicating.”
The university also recognizes that they’re recruiting nontraditional students who may have different needs than “typical” college freshmen.
“We have invested in these students by providing a student support specialist that does sort of a wraparound with them,” Kaul said. “We know that they don’t just come with educational needs. They have all the social determinants of health against them. We need to help support them so that they can be successful in this program. We feel really, really fortunate to have that position to help with that.”
For Arcelay, that’s been key to making it through the first year-plus.
“This program does not leave you alone,” she said. “Which was a lot of my hesitation. You’re usually on your own doing it. It’s so hard, and you don’t have anyone but maybe your classmates to help you. But here the professors are hands on. It’s a great program. They know that we are usually non traditional. And they’re there for us.”
If you want to know more about nursing programs, you can visit sites like https://www.calc.edu/programs/practical-nursing/.
“If you don’t have the educators …”
By creating a grassroots, community-based two-year nursing program, Carroll University is looking to remove barriers for many folks who could have long, successful careers in nursing.
But that effort can only go so far with another massive shortage in the way: a shortage of nursing educators.
“We have a lot of people that want to come into the profession. But we also don’t have enough nurse educators to teach them,” Kaul said. “If you don’t have the educators, you don’t have the nurses.”
Kaul said there are many perks to transitioning out of nursing and into nursing education – better hours, fewer physical demands. But the salaries are significantly lower.
Many people wishing to enter the profession without enough people to educate them leads to a bottleneck of nursing education programs becoming more competitive than they should be.
“Every nursing school is competitive,” said Celise Jones, a sophomore at UW-Green Bay pursuing a bachelor’s degree in nursing. “One of the prerequisite courses that you might have to take, before you get into the nursing program, you may have to fail a couple times. A lot of people I know want to do nursing, but it’s just so hard to get through it.”
Jones said she feels some of the nursing curriculum could be tailored more closely to the specific needs of nursing.
For example, she said she understands the need to learn the chemistry involved in pharmacology – the makeup of medications – but “I don’t really need to know the periodic table.”
For her part, Arcelay said she knows why it has to be tough.
“You have to want it. It’s not all what people think it is, when you walk in the door, it’s not just as easy as you think. I wouldn’t just want anyone taking care of my family either,” she said. “At the end of the day, you want it to be tough, you want it to be something that has some backbone to it, because (in the nursing profession) it’s life or death, right? So at the end of the day, I get it, and it is tough, it is hard, but there’s a reason for it. If you want it bad enough, I think that you just have to stick through it, you have to give it a time, you have to give it the effort.”
“To make that difference”
In addition to getting more prospective nurses through the education system and into jobs, it’s important to retain people in those jobs – an effort that begins with self care.
“It can be draining, but also at the same time, it is rewarding,” said Jones, who got some experience in the field in a CNA training program before the pandemic began. “I think for me, in my mindset, I have to also take care of myself, as well, which I’m still learning … it’s such a stressful job, no matter if you’re in a pandemic or not.”
If one nursing job burns you out, it’s perfectly acceptable and possible to find another, Kaul said.
“Nursing is just so vast, and it’s different areas you can go into, that you can never get bored,” Kaul said, noting that changing paths within the profession is not frowned upon.
“I didn’t know the wide world of nursing” before beginning the Carroll program, Arcelay said. “There’s just hundreds of possibilities.”
Despite the difficulties, especially through the pandemic, everyone we spoke with said the caring profession is worth the effort.
“I love the interaction with patients,” Jones said. “I like the team building.”
“I think that’s what’s so beautiful about nursing is I can be both the science, and I can be the art in my job,” Kaul said. “Sitting next to somebody going through cancer treatment is such a privilege … to be there holding their hand through that, what a wonderful thing to make a difference in someone’s life. I think we’re all here on this Earth to make differences. I can’t think of a better profession than nursing to make that difference.”
The best way to protect yourself and your community from COVID-19 is to get vaccinated and stay current on boosters. Click here for more infomation.